Презентація з англійської мови Disease : Rheumatoid arthritis
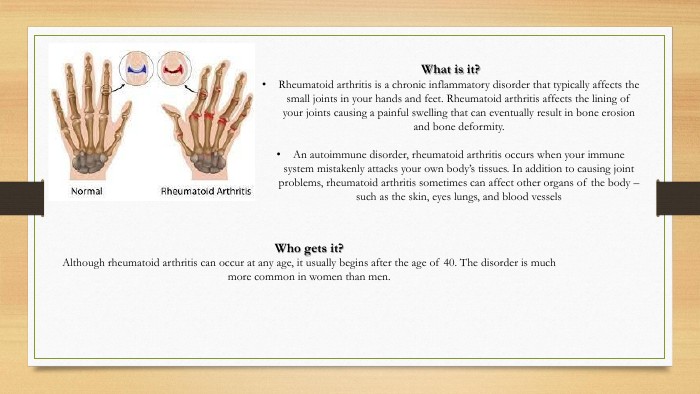

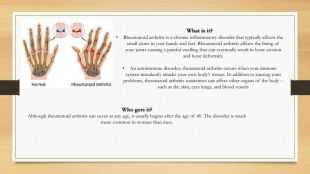
What is it?Rheumatoid arthritis is a chronic inflammatory disorder that typically affects the small joints in your hands and feet. Rheumatoid arthritis affects the lining of your joints causing a painful swelling that can eventually result in bone erosion and bone deformity. An autoimmune disorder, rheumatoid arthritis occurs when your immune system mistakenly attacks your own body’s tissues. In addition to causing joint problems, rheumatoid arthritis sometimes can affect other organs of the body – such as the skin, eyes lungs, and blood vessels. Who gets it?Although rheumatoid arthritis can occur at any age, it usually begins after the age of 40. The disorder is much more common in women than men.
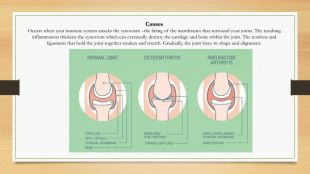
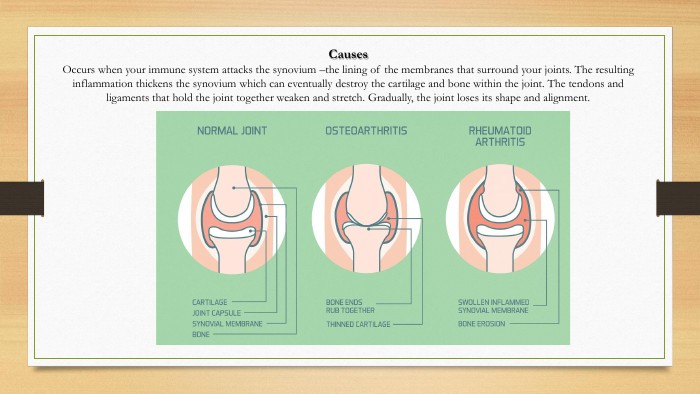
Causes. Occurs when your immune system attacks the synovium –the lining of the membranes that surround your joints. The resulting inflammation thickens the synovium which can eventually destroy the cartilage and bone within the joint. The tendons and ligaments that hold the joint together weaken and stretch. Gradually, the joint loses its shape and alignment.
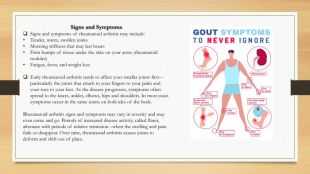
Signs and Symptoms. Signs and symptoms of rheumatoid arthritis may include: Tender, warm, swollen joints. Morning stiffness that may last hours. Firm bumps of tissue under the skin on your arms (rheumatoid nodules)Fatigue, fever, and weight loss. Early rheumatoid arthritis tends to affect your smaller joints first –particularly the joints that attach to your fingers to your palm and your toes to your feet. As the disease progresses, symptoms often spread to the knees, ankles, elbows, hips and shoulders. In most cases symptoms occur in the same joints on both ides of the body. Rheumatoid arthritis signs and symptoms may vary in severity and may even come and go. Periods of increased disease activity, called flares, alternate with periods of relative remission –when the swelling and pain fade or disappear. Over time, rheumatoid arthritis causes joints to deform and shift out of place.
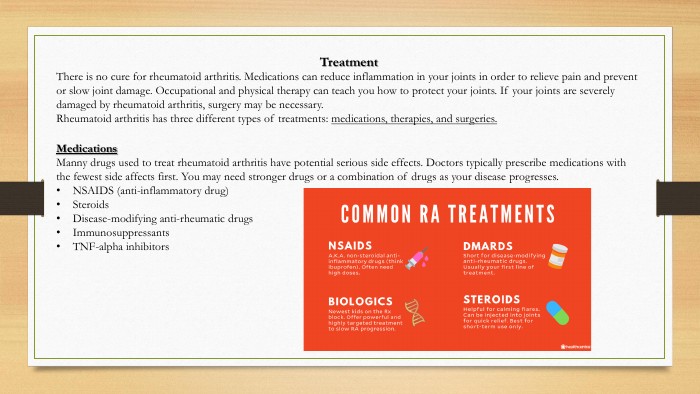
Treatment There is no cure for rheumatoid arthritis. Medications can reduce inflammation in your joints in order to relieve pain and prevent or slow joint damage. Occupational and physical therapy can teach you how to protect your joints. If your joints are severely damaged by rheumatoid arthritis, surgery may be necessary. Rheumatoid arthritis has three different types of treatments: medications, therapies, and surgeries. Medications. Manny drugs used to treat rheumatoid arthritis have potential serious side effects. Doctors typically prescribe medications with the fewest side affects first. You may need stronger drugs or a combination of drugs as your disease progresses. NSAIDS (anti-inflammatory drug)Steroids. Disease-modifying anti-rheumatic drugs. Immunosuppressants. TNF-alpha inhibitors
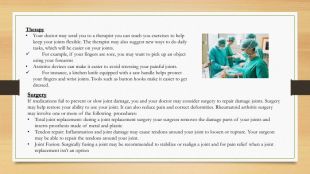
Therapy. Your doctor may send you to a therapist you can teach you exercises to help keep your joints flexible. The therapist may also suggest new ways to do daily tasks, which will be easier on your joints. For example, if your fingers are sore, you may want to pick up an object using your forearms. Assistive devices can make it easier to avoid stressing your painful joints. For instance, a kitchen knife equipped with a saw handle helps protect your fingers and wrist joints. Tools such as button hooks make it easier to get dressed. Surgery. If medications fail to prevent or slow joint damage, you and your doctor may consider surgery to repair damage joints. Surgery may help restore your ability to use your joint. It can also reduce pain and correct deformities. Rheumatoid arthritis surgery may involve one or more of the following procedures: Total joint replacement: during a joint replacement surgery your surgeon removes the damage parts of your joints and inserts prosthesis made of metal and plastic. Tendon repair: Inflammation and joint damage may cause tendons around your joint to loosen or rupture. Your surgeon may be able to repair the tendons around your joint. Joint Fusion: Surgically fusing a joint may be recommended to stabilize or realign a joint and for pain relief when a joint replacement isn’t an option
Whо is a Rheumatologist?A rheumatologist is an internist or pediatrician who received further training in the diagnosis (detection) and treatment of musculoskeletal disease and systemic autoimmune conditions commonly referred to as rheumatic diseases. These diseases can affect the joints, muscles, and bones causing pain, swelling, stiffness, and deformity. After they receive their MD or OD, rheumatologists spend three years training to become an internist or pediatrician, followed by two to three more years in a rheumatology fellowship. Like all physicians, they are lifelong learners who take continuing medical education to keep up to date in their field — especially with the emergence of new and complex treatments such as biologics. Rheumatologists treat many similar joint diseases as orthopedists, but they don’t do surgery. Many common diseases that they treat include rheumatoid arthritis, gout, lupus, osteoarthritis, and chronic back pain
Education and training requirements. According to the College of Rheumatology, before a rheumatologist can start treating patients, they must fulfill the following education and training requirements:graduate from a medical schoolcomplete a residency programparticipate in a rheumatology fellowship. After completing a “Rheumatology fellowship program,” they must pass a board examination and receive a certificate to practice rheumatology. Rheumatologists must also participate in continuing education courses throughout their careers. A rheumatologist can choose to treat specific rheumatic conditions or narrow their focus to a particular area, or subspecialty, within rheumatology. Subspecialties in the field of rheumatology include:autoimmune and inflammatory conditionsnoninflammatory degenerative joint conditionssoft tissue diseaseschronic painmetabolic disorders that affect the bonepediatric or juvenile rheumatic conditions
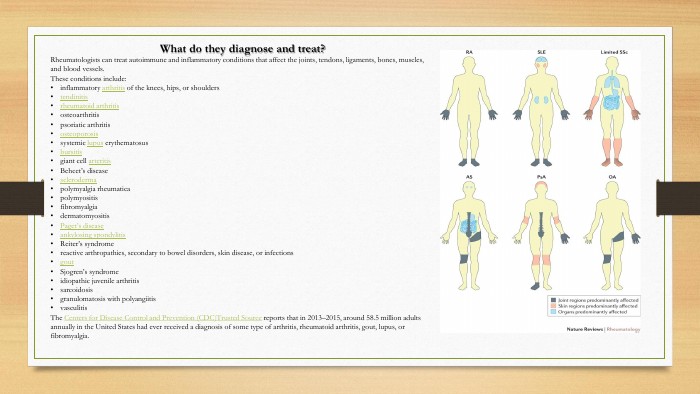
What do they diagnose and treat?Rheumatologists can treat autoimmune and inflammatory conditions that affect the joints, tendons, ligaments, bones, muscles, and blood vessels. These conditions include:inflammatory arthritis of the knees, hips, or shoulderstendinitisrheumatoid arthritisosteoarthritispsoriatic arthritisosteoporosissystemic lupus erythematosusbursitisgiant cell arteritis. Behcet’s diseasesclerodermapolymyalgia rheumaticapolymyositisfibromyalgiadermatomyositis. Paget’s diseaseankylosing spondylitis. Reiter’s syndromereactive arthropathies, secondary to bowel disorders, skin disease, or infectionsgout. Sjogren’s syndromeidiopathic juvenile arthritissarcoidosisgranulomatosis with polyangiitisvasculitis. The Centers for Disease Control and Prevention (CDC)Trusted Source reports that in 2013–2015, around 58.5 million adults annually in the United States had ever received a diagnosis of some type of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia.
What procedures do they perform?Rheumatologists perform examinations and procedures that help them diagnose and treat rheumatic conditions. These procedures include: Physical exams. A rheumatologist usually performs a complete physical exam when they see a person for the first time or when they want to monitor the effects of a current treatment program. During a physical exam, a rheumatologist will assess the person’s overall physical condition by checking their pulse, listening to their lungs and heart, and feeling for swollen lymph nodes. They will spend extra time examining areas where people report feeling pain or stiffness. They might ask a person to bend, flex, or stretch these areas. They will also look at joints on both sides of the body to compare size, the intensity of inflammation, range of motion, and function. People with arthritis can experience symptoms in one or more joints on one side of the body, while others may notice pain and stiffness in one or more joints on both sides of the body. A rheumatologist will also review a person’s medical history, current medical conditions, and family history during this comprehensive examination.
Diagnostic testing. Rheumatologists diagnose systemic inflammatory diseases and musculoskeletal conditions. They use a variety of tests to identify the underlying cause of a person’s symptoms. Some potential causes of inflammation include:environmental exposuresgeneticsinfectionsautoimmune conditionsabnormal uric acid metabolism. A rheumatologist can also diagnose conditions that cause bone or cartilage loss, including osteoporosis and osteoarthritis. Imaging tests. A primary care physician or rheumatologist can use different imaging tests to look for signs of joint damage. Some imaging tests they may conduct include: X-ray. Ultrasound. MRI scan. CT scan
Laboratory testing. Laboratory testing involves taking blood, urine, or joint fluid samples for further analysis. A rheumatologist can use lab test results to identify signs of inflammation and infections, such as higher-than-normal levels of inflammatory reactants, antibodies, or white blood cells. They can also perform tests to look for specific genetic markers that may increase their risk of specific autoimmune or inflammatory conditions. For instance, according to the American College of Rheumatology, around 60–70% of people with European ancestry and rheumatoid arthritis carry a gene called HLA-DR4. The HLA system regulates the immune system. In recent years, researchers have also discovered several genetic markers associated with ankylosing spondylitis. These include HLA-B27, ARTS 1, and IL23 R.
Treating rheumatic conditions. Rheumatologists can suggest and provide treatments for many rheumatic conditions. They can also offer consultation on many cases. Treatments they may recommend can include the following: Joint injections and aspirations. A rheumatologist can treat joint inflammation and pain by injecting an anti-inflammatory medication, such as corticosteroid, directly into the affected joint, or they can aspirate the joint to relieve pressure. When a rheumatologist aspirates a joint, they use a needle attached to a syringe to remove the excess joint fluid. They use joint aspiration to reduce patients’ joint swelling and pain and analyze the joint fluid as a part of the diagnostic protocol. Medications. A rheumatologist might prescribe disease-modifying antirheumatic drugs. These drugs lower immune system activity or slow down the progress of rheumatic conditions. Nonsteroidal anti-inflammatory drugs — such as ibuprofen, naproxen, meloxicam, and aspirin — can also help relieve joint inflammation and reduce pain.
When to see a rheumatologist. Many people experience occasional joint and muscle pain. However, people who notice pain or stiffness that does not improve within a few weeks may want to consider visiting their primary care physician. A primary care physician will evaluate a person’s symptoms and decide whether to refer them to a rheumatologist for further examination. A primary care physician may refer an individual to a rheumatologist when:they have made a diagnosis of or suspect that a person has a systemic inflammatory condition, and they want a second opinionthe person has symptoms of rheumatism and a family history of rheumatic diseasethe person’s symptoms improve after treatment but return if they stop taking medicationthe person’s symptoms do not respond to treatment or worsen over timethe person develops unexpected complications, such as unexplained fever, rash, or fatiguethe person has unusual laboratory test results
Summary. Rheumatologists are medical doctors who specialize in diagnosing and treating rheumatic diseases, including arthritis and autoimmune conditions. A rheumatologist can diagnose rheumatic conditions by taking a comprehensive medical history, performing a complete physical exam, and examining laboratory and imaging test results. They can also perform various procedures — including lumbar punctures, bursal injections, joint injections, and joint aspiration — to help diagnose and treat joint conditions. Thank you for your attention
про публікацію авторської розробки
Додати розробку